Subro Identifications
Process Overview
Claims are evaluated for subrogation potential based on several key factors:
- Claim Status
- Loss Details
- Claim Amount
- Location Information
- Deductible Information
- Statute Date
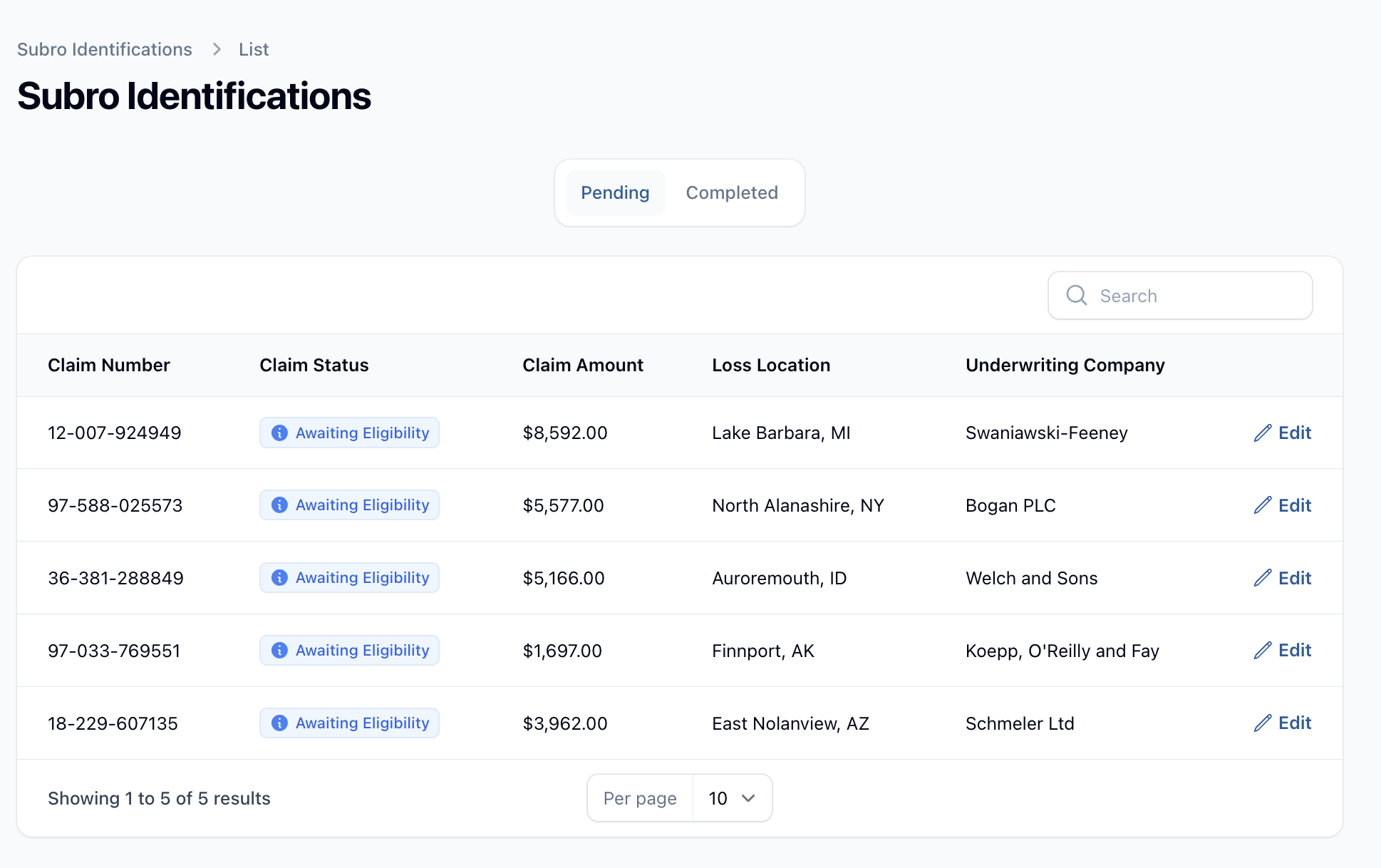
Workflow
- Claims enter the system and are automatically queued for subro review if they meet initial criteria
- Claims appear in the Subro Identifications dashboard for review
- Analysts review each claim and make one of the following decisions:
- Approve for Subrogation
- Decline Subrogation
- Request Additional Information
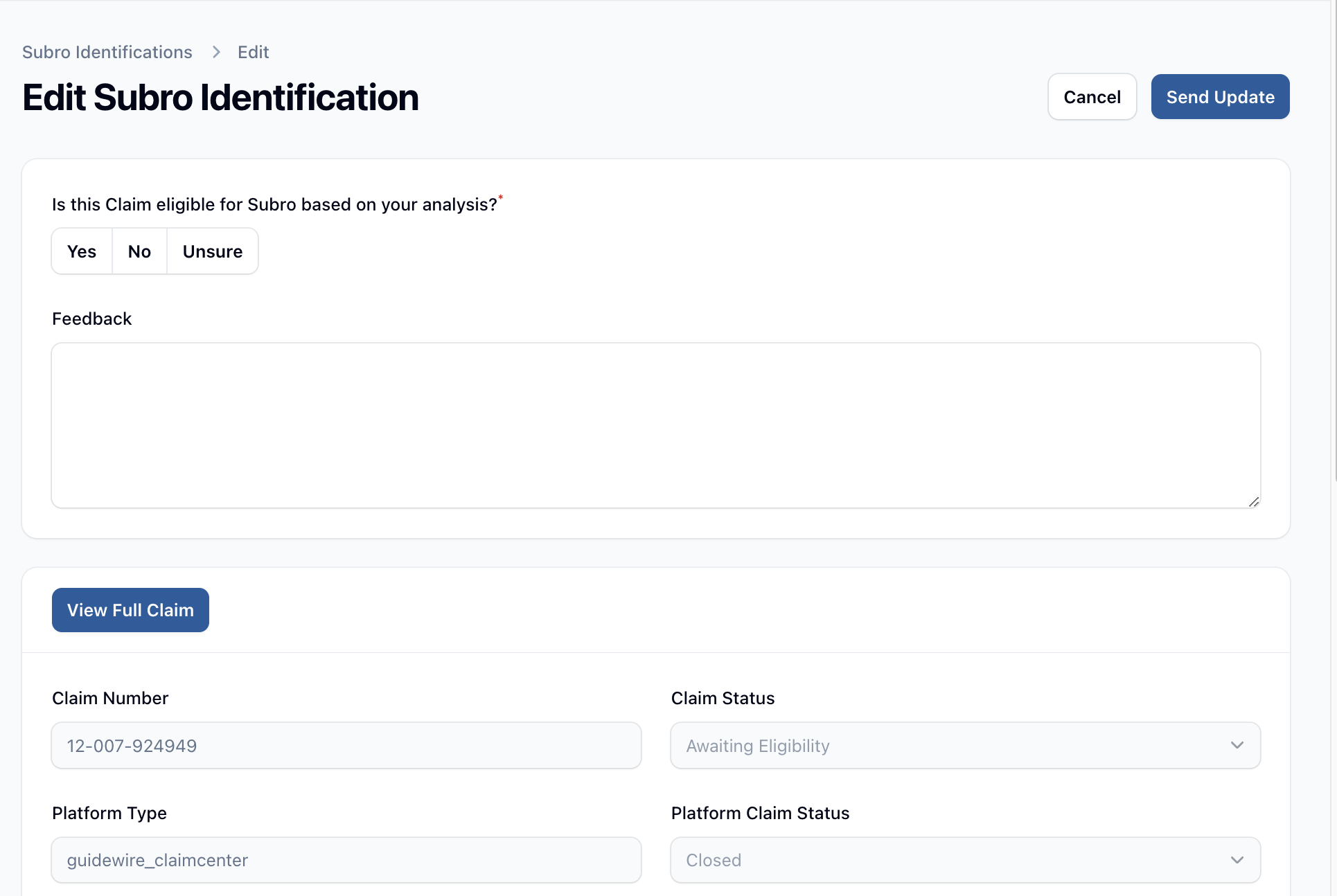
Review Interface
The review interface provides analysts with comprehensive claim information including:
- Basic claim details (claim number, status, amount)
- Loss information (timestamp, location, description)
- Underwriting details
- Deductible information
- Statute limitations
Decision Making
Analysts can:
- Make a subrogation eligibility decision
- Provide detailed feedback explaining their decision
- View the full claim record if additional information is needed
Integration
When a decision is made:
- The system updates the claim status
- The decision is synchronized with the carrier's system (Guidewire)
- The claim moves to the appropriate next stage in the workflow
Tracking
The system maintains:
- A count of pending subro identifications
- Complete decision history
- Feedback and notes for each decision
- Full audit trail of all actions taken
Status Management
Claims can have the following subro identification statuses:
- Pending: Awaiting review
- Completed: Decision has been made and recorded